Read and report vaccine reactions, harassment and failures.
Meningococcal Disease & Vaccine Information
Meningococcal: The Disease
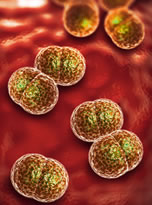
Meningococcal disease is a bacterial infection caused by the bacteria Neisseria meningitidis (N. meningitidis). There are thirteen identified types (serogroups) of N. meningitidis or meningococci, with six causing epidemics resulting in invasive meningococcal disease. Meningitis is the most common form of invasive meningococcal disease, accounting for about 75 percent of all cases.
Symptoms of meningitis usually appear between three and seven days after exposure to the meningococcal bacteria. At first, symptoms may appear mild and similar to cold or flu symptoms, such as headache, fever, aches, and pains. As the illness progresses, additional symptoms may arise, including skin rash, severe headache, stiff neck, nausea, vomiting, inability to look at bright lights, mental confusion and irritability, extreme fatigue/sleepiness, convulsions, and unconsciousness. In babies, symptoms may include a high-pitched moaning cry, difficulty or refusal to feed, and bulging of the fontanel (the soft area on the top of the head). Learn more about Meningococcal…
Meningococcal Vaccine
There are currently seven FDA licensed meningococcal vaccines in the U.S. However, two vaccines, Menactra and Menomune, are no longer produced. In total, these vaccines target five of the 13 meningococcal serotypes. Menveo, MenQuadfi, and PENBRAYA are conjugate vaccines that target serogroups A, C, Y and W-135. BEXSERO and TRUMENBA are recombinant vaccines that target serogroup B.
The CDC recommends that children 11 to 12 years of age receive the first dose of ACWY meningococcal vaccine conjugate, and a booster dose at age 16. For individuals at age 16 or older, vaccines for all currently available serogroups (A, C, W, Y and B) are recommended by the CDC. The CDC also recommends that high risk children between 2 months and 10 years and high-risk adults be vaccinated with meningococcal conjugate vaccine.Learn more about Meningococcal vaccine…
Meningococcal Quick Facts
Meningococcal
- Meningococcal disease is a serious and potentially life-threatening infection caused by the bacteria Neisseria meningitides. Most frequently, the illness can result in inflammation of the meninges of the brain (meningitis) and a serious bloodstream infection (septicemia/meningococcemia). Invasive meningococcal disease can also present as arthritis and pneumonia.
- Meningococcal disease is not easily spread and requires one to be susceptible to the infection and to have regular close contact with a person who is colonizing the bacteria. Between 10-20 percent of individuals are asymptomatic carriers and colonize the bacteria that causes meningococcal disease in the back of their throats. Natural community immunity contributes significantly to low disease incidence. Research shows that about 20 to 40 percent of Americans are asymptomatically colonizing meningococcal organisms in their nasal passages and throats. This colonization boosts an individual’s innate immunity to invasive meningococcal infection throughout life. The CDC has recognized high levels of innate community immunity and noted that the majority of Americans will experience asymptomatic infection as children or young adults without complications and develop protective bactericidal antibodies against meningococcal disease.
- Meningococcal rates are low in the U.S. and have steadily declined since the 1990’s. In 2020, there were approximately 235 cases in the U.S. Of these cases 26 percent were unknown and ungroupable serotypes with 20 percent occurring in children too young to be vaccinated. For 2020, 23 death were reported, or less than ten percent of cases. Individuals most at risk for contracting meningococcal disease are infants, adolescents, young adults and seniors. Continue reading quick facts…
Meningococcal Vaccine
- The CDC states that individuals receiving meningococcal vaccines may experience mild side effects such as pain or redness at the injection site, headache, fatigue, muscle and joint pain, fever, chills, nausea, and diarrhea. Additionally, the CDC warns that persons receiving any vaccine may collapse (faint), experience a severe allergic reaction, and even serious injury and death. Serious adverse events associated with meningococcal vaccines include anaphylaxis, wheezing, upper airway swelling, difficulty breathing, hypotension, itching, hives, lymph node swelling, Guillain-Barre syndrome, convulsions, facial palsy, vasovagal syncope, paresthesia, transverse myelitis, acute disseminated encephalomyelitis, extensive swelling of the injected limb and injection site.
- Meningococcal B vaccines have not been given a routine recommendation by the CDC due to several factors. These factors included the high number of vaccinations that would be required to prevent a single case of the disease, low rates of disease, cost of the vaccine, lack of efficacy and safety data, and the possibility of serious adverse vaccine reactions exceeding the number of cases prevented.
- In 2020, 85.7 percent of college students (18-24 years) and 69.2 percent of persons not attending college (18-24 years) had received at least one dose of MenACWY vaccine. For this same age group and college status, 14.3 percent of college students and 18.2 percent of persons not attending college had received at least one dose of MenB vaccine. Continue reading quick facts…
NVIC encourages you to become fully informed about Meningococcal and the Meningococcal vaccine by reading all sections in the table of contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.



