Read and report vaccine reactions, harassment and failures.
Haemophilus Influenzae Type B (HIB) Disease & Vaccine Information
HIB: The Disease
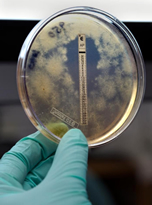
Haemophilus influenzae type b (Hib) is a bacterial infection that can cause severe illnesses in children that include meningitis, epiglottitis, pneumonia, arthritis, and cellulitis. Hib meningitis, an infection of the membranes covering the brain and one of the most serious complications of Hib, may occur following an upper respiratory illness. Infection can spread from the sinuses and lungs into the bloodstream and to the brain causing meningitis. HIB is transmitted by direct contact with respiratory secretions and enters the body through the upper respiratory tract. In most cases, Hib can remain in the mouth and nose for up to several months, without causing illness. In general, HIB is considered to be minimally contagious, however, if a person has close contact to someone who is infected with or is carrying H. influenzae, transmission can occur. Learn more about Hib…
HIB Vaccine
There are five Haemophilus influenzae type b vaccines available for use by the United States Food and Drug Administration (FDA) and recommended by the Centers for Disease Control (CDC). The CDC has approved Hib vaccine for use in children at 2, 4, 6 and 12-15 months of age. . Learn more about HIB vaccine…
HIB Quick FactsHaemophilus Influenzae Type B (Hib)
- Haemophilus influenzae type b (Hib) is a bacterial infection that can cause severe illnesses in children, including meningitis, epiglottitis, pneumonia, arthritis, and cellulitis;
- In general, the transmission of Hib is considered to be limited and when it occurs, it usually affects only close contacts such as household members. Prior to the introduction of the Hib vaccine, most children acquired natural immunity to Hib by the time they were 5 or 6 years old. Continue reading quick facts…
HIB Vaccine
- All infants and children who participated in Hib vaccine pre-licensing clinical trials also received other vaccines in addition to the Hib vaccine. As a result, it is not possible to determine the specific adverse reaction to monitor for following Hib vaccination. The administration of multiple vaccines also makes it difficult to determine the specific vaccine that might have triggered the reactions reported in both clinical studies and to VAERS.
- Mild side effects such as redness, warmth, or swelling where the shot was given have been reported in connection with administration of Hib vaccines. Systemic reactions, such as fever and irritability can also occur. Severe reactions involving Hib vaccination were reported during pre-licensing clinical trials and continue to be reported to the Vaccine Adverse Events Reporting System (VAERS). These include deaths, anaphylactic reactions, asthma, pneumonia, convulsions, noninfectious encephalitis, acute pancreatitis, peripheral neuropathy, Guillain-Barre syndrome, sepsis, seizures, and cerebral edema. Continue reading quick facts...
NVIC encourages you to become fully informed about Haemophilus Influenza Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents , which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.



