Read and report vaccine reactions, harassment and failures.
Pneumococcal disease & vaccine information
Pneumococcal: The Disease
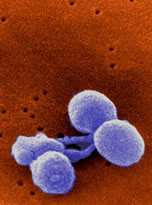
Pneumococcal disease is an infection caused by Streptococcus pneumoniae (S. pneumoniae) bacteria. Only a few of the serotypes cause the majority of pneumococcal infections but nearly all serotypes have the ability to cause serious disease. S. pneumoniae are frequently found in the respiratory tract and up to 90 percent of healthy people may have the bacteria present in the nasopharynx (upper area of the throat behind the nose). Between 20 and 60 percent of all school children may also carry the bacteria.
Most pneumococcal infections are mild, however, serious illness can occur. S. pneumoniae can cause several types of infections, including pneumonia, ear infections, sinus infections, bloodstream infections (bacteremia) and meningitis. Less commonly, S. pneumoniae can cause bacterial bone and joint infections, pericarditis, endocarditis, and peritonitis. Learn more about Pneumococcal…
Pneumococcal Vaccine
The U.S. Food and Drug Administration (FDA) and U.S. Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control (CDC) has approved two different pneumococcal containing shots. There are different rules for use of these vaccines by different aged groups.
Prevnar 13 is a 13-valent pneumococcal conjugate vaccine (PCV) manufactured by Wyeth (Pfizer) pharmaceuticals, containing Streptococcus pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F and 23F. Prevnar 13 does not protect against infection and disease caused by Streptococcus pneumoniae strains not present in the vaccine. Prevnar 13 is approved for varying uses in children, teenagers and adults.
PNEUMOVAX23 is a pneumococcal polysaccharide vaccine (PPSV) manufactured by Merck and contains Streptococcus pneumoniae serotypes 1, 2, 3, 4, 5, 6B, 7F, 8, 9N, 9V, 10A, 11A,12F, 14, 15B, 17F, 18C, 19F, 19A, 20, 22F, 23F, and 33F. Pneumovax 23 does not protect against infection and disease caused by Streptococcus pneumoniae strains not present in the vaccine. PNEUMOVAX23 is approved for use in adults 50 years of age or older and in children 2 and older who are at increased risk for pneumococcal disease. Learn more about Pneumococcal vaccine…
Pneumococcal Quick Facts
Pneumococcal
- Symptoms of pneumococcal infection include sudden onset of fever and fatigue, sneezing and cough with mucus and shortness of breath. The infection may start with a general feeling of being unwell, a low-grade fever and a cough that doesn’t include mucus before symptoms worsen. Symptoms of pneumococcal meningitis (brain inflammation) include stiff neck (inability to touch the chin to chest without moderate to severe pain in the back of the neck and head); headache; extreme fatigue or seizures. Symptoms of otitis media include a painful ear, red or swollen eardrum, fever, and irritability.
- Pneumococcal bacteria are primarily transmitted through respiratory secretions by coughing and sneezing. Persons most at risk of developing invasive pneumococcal disease include immunocompromised individuals, smokers, persons with chronic cardiac, lung, or kidney disease, individuals without a spleen, and persons with cochlear implants or a cerebrospinal fluid leak. Children attending daycare are also at a higher risk. Continue reading quick facts…
Pneumococcal Vaccine
- The CDC recommends four doses of pneumococcal conjugate vaccine (PCV13) for infants and children, with a dose given at 2, 4, 6 and between 12 and 18 months of age. Children between 2 and 18 years who are at a higher risk of invasive pneumococcal disease are also recommended to receive one dose of PPSV23 at least 8 weeks following the most recent dose of PCV13. A second dose of PPSV23 is recommended at least 5 years following the first dose in children who are immunocompromised, HIV-positive, have sickle cell disease, or who lack a functioning spleen. PPSV23 and PCV13 are also recommended for use in immunocompromised children, adults, and seniors.
- All adults 65 years of age and older are recommended by the CDC to receive one dose of PPSV23. PCV13 can also be considered for use in healthy seniors 65 years and older but routine vaccination is no longer recommended. This recommendation was revised at the June 2019 Advisory Committee on Immunization Practices (ACIP) when data presented found limited benefit to vaccinating all seniors with PCV13 vaccine. Continue reading quick facts…
NVIC encourages you to become fully informed about Pneumococcal and the Pneumococcal vaccine by reading all sections in the Table of Contents below, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.



