Read and report vaccine reactions, harassment and failures.
HIB: The Disease
Haemophilus influenzae type b (Hib) is a bacterial infection that can cause severe illnesses in children that include meningitis, epiglottitis, pneumonia, arthritis, and cellulitis. Hib meningitis, an infection of the membranes covering the brain and one of the most serious complications of Hib, may occur following an upper respiratory illness. Infection can spread from the sinuses and lungs into the bloodstream and to the brain causing meningitis. HIB is transmitted by direct contact with respiratory secretions and enters the body through the upper respiratory tract. In most cases, Hib can remain in the mouth and nose for up to several months, without causing illness. In general, HIB is considered to be minimally contagious, however, if a person has close contact to someone who is infected with or is carrying H. influenzae, transmission can occur. Learn more about Hib…
HIB Vaccine
There are five Haemophilus influenzae type b vaccines available for use by the United States Food and Drug Administration (FDA) and recommended by the Centers for Disease Control (CDC). The CDC has approved Hib vaccine for use in children at 2, 4, 6 and 12-15 months of age. . Learn more about HIB vaccine…
HIB Quick FactsHaemophilus Influenzae Type B (Hib)
- Haemophilus influenzae type b (Hib) is a bacterial infection that can cause severe illnesses in children, including meningitis, epiglottitis, pneumonia, arthritis, and cellulitis;
- In general, the transmission of Hib is considered to be limited and when it occurs, it usually affects only close contacts such as household members. Prior to the introduction of the Hib vaccine, most children acquired natural immunity to Hib by the time they were 5 or 6 years old. Continue reading quick facts…
HIB Vaccine
- All infants and children who participated in Hib vaccine pre-licensing clinical trials also received other vaccines in addition to the Hib vaccine. As a result, it is not possible to determine the specific adverse reaction to monitor for following Hib vaccination. The administration of multiple vaccines also makes it difficult to determine the specific vaccine that might have triggered the reactions reported in both clinical studies and to VAERS.
- Mild side effects such as redness, warmth, or swelling where the shot was given have been reported in connection with administration of Hib vaccines. Systemic reactions, such as fever and irritability can also occur. Severe reactions involving Hib vaccination were reported during pre-licensing clinical trials and continue to be reported to the Vaccine Adverse Events Reporting System (VAERS). These include deaths, anaphylactic reactions, asthma, pneumonia, convulsions, noninfectious encephalitis, acute pancreatitis, peripheral neuropathy, Guillain-Barre syndrome, sepsis, seizures, and cerebral edema. Continue reading quick facts...
NVIC encourages you to become fully informed about Haemophilus Influenza Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents , which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
What is Haemophilus Influenza Type B (HIB)?
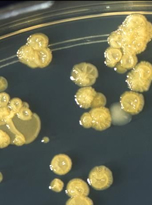
Haemophilus influenzae (H. influenzae) is a small gram-negative coccobacillus found only in humans and can be either encapsulated (typeable) or unencapsulated (nontypeable). Typeable H. influenzae contain a polysaccharide capsule and are identified and labeled with letters a through f. Strains that do not have a polysaccharide capsule are referred to as nontypeable. Current H. influenzae vaccines target only H. influenzae type b, which was believed to be the cause of 95 percent of all H. influenzae infections in the pre-vaccine era. Hib infections are more likely to occur between September and December and again between March and May.
H. influenzae type b (Hib) is transmitted by direct contact with respiratory secretions and enters the body through the upper respiratory tract. While uncommon, H. influenzae type b and other types of H. influenzae infections can also be transmitted through the birth canal from an infected mother to her newborn baby. In most cases, Hib can remain in the mouth and nose for up to several months without causing illness. If Hib enters the bloodstream it becomes invasive and cause serious infections including meningitis, pneumonia, bacteremia, epiglottis, cellulitis, septic arthritis, osteomyelitis, otitis media, pericarditis, and endocarditis.
A diagnosis of H. influenzae, including H. influenzae type b, is made by the laboratory testing of bodily fluids such as blood and spinal fluid.
Prior to the introduction of the Hib vaccine in the mid-1980’s, H. influenzae type b was responsible for most cases of meningitis, a serious infection of the membranes that cover the spinal cord and brain, which is the most common clinical presentation of invasive disease. Before Hib vaccines became available, infections occurred nearly exclusively in children under the age of five, with the majority of infections occurring in children younger than eighteen months. Of note, Navajo and Native Alaskan Americans were found to have higher rates of the disease. H.influenzae invasive disease did not become a nationally notifiable disease until 1991, six years after the first Hib vaccines became available for use in the United States.
Since the introduction of Hib vaccines, Hib meningitis has become more common in adults than in children. While the CDC reports a nearly 99 percent decrease in Hib invasive disease among children 5 years of age and younger, adults, especially seniors over the age of 65, have become more susceptible to the infection. A 2011 published study on H. influenzae infections in Utah found that between 1998 and 2008, over 50 percent of H. influenzae infections and 67 percent of H. influenzae related deaths occurred in adults over the age of 65.
In the United States, before Hib vaccines became available, approximately two-thirds of all cases of Hib invasive disease affected infants and children under 15 months of age and 85 percent of cases occurred in children under the age of five. Following the introduction of the Hib vaccine, the burden of invasive H. influenzae disease has shifted from children to adults, and most particularly seniors over the age of 65. A 2011 published study found that between 1998 and 2008, 51 percent of invasive H. influenzae cases involved adults over the age of 65. Death rates from H. influenzae disease were also found to be significantly higher among seniors over age 65, with 67 percent of infections resulting in death.
While invasive disease caused by H. influenzae type b (Hib) has decreased, invasive disease by non-b and nontypeable H. influenzae have increased. Non-b type infections, such as H. influenzae type a, can cause invasive disease with complications similar to Hib and nontypeable H. influenzae invasive illness, while most commonly associated with infections such as conjunctivitis, otitis media, sinusitis, and pneumonia, still has the potential to cause serious invasive H. influenzae disease. Hib vaccines target only H. influenzae type b and offers no protection against any other type of H. influenzae infection.
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
Is Hib contagious?

H. influenzae type b (Hib), along with all H. influenzae types, including both non-b and nontypeable H. influenzae, are contagious. H. influenzae is spread by direct contact with the respiratory secretions of someone who is a carrier or is infected with H. influenzae. Less commonly, infection can be spread to newborn infants if they come into contact with genital or amniotic fluid from an infected mother during the birth process.
H. influenzae enters the body through the upper respiratory tract, and can remain there for several months without causing illness. Nontypeable strains of H. influenzae colonize in the respiratory tract of approximately 75 percent of healthy adults. Currently, Hib is believed to colonize in the back of the throat in three to five percent of children. In some individuals, the organism causes an invasive infection such as pneumonia or meningitis. Although it is not known how H. influenzae enters the bloodstream, it is possible that a co-existing viral or mycoplasma infection of the upper respiratory tract may be a contributing factor.
In general, H. influenzae disease is considered to be minimally contagious, however, if a person has close contact to someone who is infected with or is carrying H. influenzae, transmission can occur. Hib has the potential to spread quickly in populations in enclosed quarters, such as families, institutional settings, and daycare centers. Prior to the introduction of Hib vaccines in the United States, health officials had identified a seasonal pattern to Hib, with the first peak between the months of September and December, and the second peak between March and May.
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
What is the History of Hib in America and Other Countries?
Haemophilus influenzae was first identified by Robert Pfeiffer in 1892 during an epidemic of influenza. At this time, it was believed that this bacteria was responsible for influenza. However, in 1933, influenza was determined to be caused by a virus, and H. influenzae found to be a secondary infection.
In the 1930’s, Margaret Pittman identified the two distinct types of H. influenzae, the encapsulated and unencapsulated strains. Pittman found six unique types of encapsulated strains of H. influenzae, labeling them as strains a to f, while noting type b to be the most prevalent strain found in both the blood and cerebrospinal fluid (CSF) samples that were collected. The unencapsulated strains of H. influenzae were attributed to mucosal surface infections such as conjunctivitis, otitis media, sinusitis, and bronchitis.
In December of 1982, three years prior to the introduction of the first Hib vaccines, the CDC reported invasive H. influenzae to be the leading cause of meningitis in the United States, and responsible for an estimated 8,000 to 11,000 infections per year, and fatal in three to seven percent of all cases. Infection rates were highest in children under the age of one and decreased consistently thereafter. It was also estimated that an additional 6,000 H. influenzae cases resulted in other forms of invasive disease that included bacteremia, cellulitis, epiglottis, and pneumonia. H. influenzae, however, was not a reportable disease in the United States until 1991, and infection rates were estimates tabulated from different sources throughout the country.
In 1991, the first year invasive H. influenzae became a nationally notifiable disease in the United States, there were 2,764 reported cases, with over half of the cases impacting children under the age of five. A 1998 CDC published report examining H. influenzae disease in infants and children found that in 1996-1997, of the 144 children diagnosed with Hib invasive disease, 27 had completed the recommended three-dose primary series (nearly 19 percent), and 14 (almost 10 percent) had also received a booster dose.
Between 1998 and 2000, there were 3,901 reported cases of H. influenzae, with 824 cases reported in children under the age of five. Of the 824 cases affecting children under the age of five, only 197 (24 percent) were confirmed to be the result of H. influenzae type b. One hundred and eleven of the 197 H. influenzae type b cases affected children over the age of 6 months of age and eligible to have completed the primary three doses of Hib vaccine. Of the 111 children, 35 percent had completed the primary Hib vaccine series, and over half of these children had also received a booster dose.
In 2010, there were 3,151 reported cases of H. influenzae disease, with 446 cases reported in children under the age of five. In children under the age of five, only 23 cases were confirmed as H. influenzae type b. The remaining cases were determined to be a combination of unknown and non-b serotype H. influenzae.
The burden of invasive H. influenzae disease has shifted from children to adults, and most notably to seniors 65 years of age and older. In 2011, two published studies reported on the change in the demographics of H. influenzae, with one study in particular noting that 51 percent of H. influenzae infections and 67 percent of H. influenzae related deaths occurred in adults over the age of 65. H. influenzae type b (Hib) was found to be responsible for only 9 percent of the serotyped cases, while 43 percent of cases were attributed to nontypeable H. influenzae strains. Non-b type H. influenzae, particularly types a and f, were found to be responsible for 49 percent of cases.
In 2020, there were 2,996 reported cases of H. influenzae, with 316 reported cases impacting children under the age of five. Of the infections reported in children under five years of age, only 15 cases were confirmed as H. influenzae type b. The number of H. influenzae type b infections in persons five years of age and older is not known.
Currently, among all age groups, nontypeable H. influenzae is responsible for the majority of invasive disease and non-b type H. influenzae infections have become more prevalent than type b. Hib vaccine does not prevent invasive disease cause by nontypeable and non-b types of H. influenzae.
Globally, in 2015, there were an estimated 340,000 cases of severe H. influenzae type b infection, and 30,000 Hib related deaths. Countries noted to have the highest rate of Hib infections included China, India, South Sudan, and Nigeria. Between 2000 and 2015, deaths from Hib were reported to have dropped by 90 percent globally.
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
Can Hib cause injury and death?

Prior to the introduction of vaccines targeting H. influenzae type b (Hib), between 0.5 and 3 percent of infants and children were reported to have Hib present in the upper respiratory tract and Hib bacteria were rarely found in adults. Most children colonized Hib and developed immunity to it by the age of six as a result of being asymptomatic carriers. Currently, Hib is believed to colonize in the back of the throat of between three and five percent of children.
The presence of Hib in infants and young children infrequently results in serious invasive disease that can include:
- · Meningitis – an infection of membranes that cover the spinal cord and brain
- · Cellulitis – a serious bacterial infection of the skin
- · Epiglottitis – an infection that causes swelling of the epiglottis, with the potential to cause airway obstruction
- · Septic arthritis – an infection of the joint
- · Pneumonia – a lung infection
- · Osteomyelitis – an infection of the bone
- · Pericarditis – an infection of the sac that covers the heart
The precise mechanism in which Hib invades the bloodstream to become invasive is not known, however, it is thought that a preceding infection involving the respiratory system may play a key role. Prior to the introduction of Hib vaccines, children under the age of one accounted for approximately 60 percent of invasive Hib disease infections, with the majority of cases impacting infants between six and 11 months of age. Additionally, Hib meningitis was reported to be the most common presentation of invasive Hib disease and responsible for 50-65 percent of cases. An estimated 8,000 to 11,000 Hib meningitis cases occurred each year and three to seven percent resulted in death. Fifteen to thirty percent of survivors had long-term neurological or hearing impairments as a result of the disease.
Hib vaccine does not offer protection against any other type of H. influenzae strains, and additional types of encapsulated strains of H. influenzae can cause invasive disease similar to Hib, including meningitis. While nontypeable (unencapsulated) strains are more likely to cause illnesses such as bronchitis and otitis media in children, they also have the potential to cause serious invasive disease. Currently among all age groups, non-typeable H. influenzae is responsible for the majority of all cases of invasive H. influenzae disease. Nontypeable strains of H. influenzae are commonly found in the nasal passages of most infants, children, and adults.
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
Who is at highest risk for getting Hib?
According to the CDC, children under the age of 5 and adults over the age of 65 are most at risk for developing Hib. Additionally, Alaskan Natives and American Indians have also been found to be at higher risk for developing invasive Hib disease.
Individuals with certain pre-existing medical conditions may also be at an increased risk. These include persons with:
- HIV infection;
- Cancer who are receiving treatment such as radiation, chemotherapy or stem cell therapy;
- Asplenia;
- Sickle Cell Disease;
- A rare immune disorder known as complement or antibody deficiency syndrome that affects a person’s ability to fight infection.
Other risk factors for the development of Hib include living in crowded households, daycare attendance, the presence of younger siblings, cigarette smoke exposure, and having a lower socioeconomic status.
Currently, adults, especially seniors, over the age of 65 are at highest risk of developing invasive H. influenzae disease. While the incidence of H. influenzae type b has decreased significantly, non-b type and nontypeable H. influenzae disease continue to result in invasive disease and appear to be replacing H. influenzae type b. Hib vaccination does not provide protection against any other form of H. influenzae.
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
Who is at highest risk for suffering complications from Hib?

Asplenic patients (people without a spleen or who have dysfunctional spleens such as individuals with sickle cell anemia or celiac disease) are predisposed to the development of serious infections from Haemophilus influenzae, Neisseria meningitides, and Streptococcus pneumoniae. Persons with underlying medical conditions such as HIV infection, alcoholism, cancer, pulmonary disease, and women who are pregnant may also be at greater risk of an infection that may to lead to complications. In the case of bacterial meningitis, including H. influenzae meningitis, developing complications or dying is related to age, underlying health of the patient, severity of the disease, and timing of antibiotic therapy.
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
Can Hib be prevented and are there treatment options?
Prior to the introduction of Hib vaccines, the majority of children acquired natural immunity to Hib through asymptomatic infection by five or six years of age. Newborns were also protected during the first several months of life due to the passage of maternal antibodies through the placenta and from breastmilk.
When a child is believed to have a serious invasive disease such as H. influenzae, hospitalization is usually required. Lab testing of blood or other bodily fluids, such as cerebrospinal fluid (CSF), is required to confirm the presence of H. influenzae, and to determine the particular type.
As strains of H. influenzae have become increasingly resistant to antibiotics such as ampicillin and amoxicillin, additional antibiotics such as ceftriaxone have been indicated for use. Antibiotic therapy for at least 10 days is generally recommended. H. influenzae meningitis generally requires the use of intravenous (IV) or intramuscular (IM) antibiotics. The corticosteroid Dexamethasone is also recommended for infants and children older than two months of age. This medication can decrease inflammation and reduce the risk of neurological complications, including hearing loss associated with meningitis. Additional supportive care may be necessary to manage complications such as seizures, shock, syndrome of inappropriate antidiuretic hormone secretion (SIADH), subdural empyema (the collection of pus between the dura mater and the underlying arachnoid mater in the brain), and any secondary infections that may occur.
Treatment of H. influenzae cellulitis can included the use of either intravenous or intramuscular antibiotics until the fever decreases and the cellulitis diminishes. Often this treatment is followed by an additional 7 to 10-day course of oral antibiotics. In the case of orbital cellulitis, inpatient IV antibiotic treatment followed by one to three weeks of oral antibiotics is recommended. Surgery may also be required to drain the abscess if the swelling is severe.
H. influenzae epiglottitis often involves the maintenance of an airway by intubation or tracheostomy. An IV antibiotic such as ceftriaxone is usually recommended until the patient is able to swallow again. When indicated, intravenous antibiotics may be switched to oral antibiotics and continued for at least seven days.
Intravenous antibiotic treatment followed by two to three weeks of oral antibiotics is generally indicated in the treatment of H. influenzae arthritis. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) blood test results can help determine how long oral antibiotics should be taken. Surgery may also be required to prevent serious complications such as necrosis.
H. influenzae bacteremia precedes nearly all other forms of invasive H. influenzae infections and between 30 to 50 percent of cases will develop into a more specific infection such as meningitis, pneumonia, or cellulitis. Lumbar punctures, additional blood cultures, and chest imagining is recommended to monitor for the risk of progression. Treatment of bacteremia involves the use of parenteral antibiotics, followed by the use of oral antibiotics.
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
What is Hib vaccine?

There are five Haemophilus influenzae type b (HIB) vaccines available for use by the United States Food and Drug Administration (FDA) and recommended by the Centers for Disease Control (CDC). These include: Sanofi Pasteur's ActHIB and GlaxoSmithKline Biological’s HIBERIX, both of which are tetanus toxoid and Haemophilus b conjugate vaccines; Merck, Sharp & Dohme’s PedvaxHIB, which is a meningococcal protein and Haemophilus b conjugate; Sanofi Pasteur’s Pentacel, which consists of diphtheria and tetanus toxoids, acellular pertussis adsorbed, inactivated poliovirus, and Haemophilus b conjugate (tetanus toxoid conjugate); and MSP Vaccine Company’s VAXELIS, a 6 in 1 (hexavalent) combination vaccine containing Haemophilus influenzae type b conjugate vaccine in combination with diphtheria and tetanus toxoid and acellular pertussis (DTaP), inactivated poliomyelis (IPV), and recombinant hepatitis B vaccine. VAXELIS combines diphtheria and tetanus toxoids, acellular pertussis and inactivated poliomyelis antigens manufactured by Sanofi Pasteur with Haemophilus influenzae type b conjugate and hepatitis B recombinant vaccines, manufactured by Merck.
Haemophilus influenzae type b (HIB) vaccines do not provide any protection against invasive disease resulting from non-b type and nontypeable H. influenzae.
Links to the available HIB vaccine package inserts can be found on the HIB Quick Facts page.
ActHIB is a conjugate vaccine made by Sanofi Pasteur that is indicated for use in infants and children ages two months through five years of age for the prevention of H. influenzae type b. ActHIB vaccine is a sterile powder that requires reconstitution with 0.4% Sodium Chloride solution. The vaccine is comprised of the Haemophilus influenzae type b capsular polysaccharide (polyribosyl-ribitol-phosphate, or PRP). PRP is formed from H. influenzae type b strain 1482 that has been cultivated in a semi-synthetic growth medium and bound to tetanus toxoid. The tetanus toxin has been taken from the Harvard strain of Clostridium tetani, purified with ammonium sulfate, rendered inactive by formalin, and grown in a modified Mueller and Miller medium, a culture medium containing raw materials made from milk. During the manufacturing process, formaldehyde levels are reduced below 0.5mcg per dose and the toxoid is sterilized prior to being conjugated. The ActHIB vaccine powder and Sodium Chloride diluent do not contain any preservatives. This vaccine is administered intramuscularly.
According to the manufacturer, when ActHIB is reconstituted with saline, each dose is formulated to contain 10 mcg of purified capsular polysaccharide conjugated to 24 mcg of inactivated tetanus toxoid and 8.5% of sucrose.
HIBERIX is a conjugate vaccine made by GlaxoSmithKline that is approved for use in infants and children ages six weeks through four years of age, prior to the fifth birthday, for the prevention of Haemophilus influenzae type b. HIBERIX is a lyophilized vaccine that is reconstituted with saline and then injected into the muscle. According to the manufacturer’s product insert, HIBERIX contains Haemophilus b capsular polysaccharide (polyribosyl-ribitol-phosphate, or PRP), a high molecular weight polymer prepared from the Haemophilus influenzae type b strain 20,752 grown in a synthetic medium. The tetanus toxin in the vaccine is prepared from Clostridium tetani grown in a semi-synthetic medium, and detoxified with formaldehyde. The polysaccharide is covalently bound to the tetanus toxoid.
When reconstituted, each dose of HIBERIX is formulated to contain 10 mcg of purified capsular polysaccharide conjugated to approximately 25 mcg of tetanus toxoid, 12.6 mg of lactose, and less than or equal to 0.5 mcg of residual formaldehyde. HIBERIX does not contain preservatives and the vial stoppers of both the lyophilized powder and saline diluent do not contain latex.
PedvaxHIB is a conjugate vaccine manufactured by Merck, Sharp & Dohme Co. that is indicated for vaccination against Haemophilus influenzae type b in infants and children ages two to 71 months of age. It is a liquid conjugate vaccine with meningococcal group B outer membrane as the protein carrier. It does not need to be reconstituted, and is injected into the muscle. It is a purified polysaccharide (polyribosylribitol phosphate or PRP) of Haemophilus influenzae type b (Haemophilus b, Ross strain) covalently bound to an outer membrane protein complex of the B11 strain of Neisseria meningitides serogroup B. The covalent bonding is necessary for enhanced immunogenicity.
Each dose of Liquid PedvaxHIB is formulated to contain 7.5 mcg of Haemophilus b PRP, 125 mcg of Neisseria meningitides OMPC and 225 mcg of aluminum as amorphous aluminum hydroxyphosphate sulfate (previously referred to as aluminum hydroxide), in 0.9 percent sodium chloride. PedvaxHIB does not contain lactose or thimerosal.
Pentacel is manufactured by Sanofi Pasteur and is indicated for vaccination against diphtheria, tetanus, pertussis, poliomyelitis and Haemophilus influenzae type b in children ages six weeks through four years of age(prior to the fifth birthday). It is injected into the muscle in a 4-dose schedule, recommended to be administered at 2, 4, 6, and between 12 and 15 months. The antigenic forms in the vaccine include a mixture of two toxoids with five acellular pertussis antigens, three types of poliovirus, and Hib conjugated to tetanus toxoid. Specifically, according to the manufacturer’s product insert, each dose of Pentacel contains 15 Lf diphtheria toxoid, 5 Lf tetanus toxoid, acellular pertussis antigens, 20 mcg detoxified pertussis toxin (PT), 20 mcg filamentous hemagglutinin (FHA), 3 mcg pertactin (PRN), 5 mcg fimbriae types 2 and 3 (FIM) inactivated polioviruses (40 D-angigen units DU Type 1 Mahoney, 8 DU Type 2 MEF-1, 32 DU Type 3 Saukett) and 10 mcg PRP of Haemophilus influenzae type b. Pentacel contains the same pertussis antigens as another vaccine, Daptacel, and is manufactured by the same process as Daptacel; however, Pentacel vaccine contains twice as much detoxified PT and four times as much FHA as Daptacel.
Additional ingredients in each 0.5ml dose of Pentacel include 1.5 mg aluminum phosphate (0.33 mg aluminum) as the adjuvant, polysorbate 80 (approximately 10 ppm), less than or equal to 5 mcg residual formaldehyde, less than 50 ng residual glutaraldehyde, 3.3 mg of 2-phenoxyethanol, less than 50 ng residual bovine serum albumin, less than 4 pg of both polymyxin B sulfate and neomycin.
The Cornyebacterium diphtheria is grown in modified Mueller’s growth medium, purified by ammonium sulfate fractionation and the diphtheria toxin is detoxified with formaldehyde and diafiltered. Clostridium tetani is grown in modified Mueller-Miller casamino acid medium without beef heart infusion and the tetanus toxin is detoxified with formaldehyde then purified by ammonium sulfate fractionation and diafiltration. The tetanus and diphtheria toxoids are each adsorbed onto aluminum phosphate. The acellular pertussis antigens are produced from Bordetella pertussis cultures grown in Stainer-Scholte medium, modified by the addition of casamino acids and dimethyl-beta-cyclodextrin. PT, FHA, and PRN are isolated individually from the culture medium. FIM are removed and copurified from the bacterial cells. The pertussis antigens are purified by sequential filtration, ultrafiltration, salt precipitation and chromoatography. PT is detoxified with glutaraldehyde, FHA is treated with formaldhyde and the residual aldehydes are removed by ultrafiltration. The antigens are adsorbed individually onto aluminum phosphate.
According to the manufacturer’s product insert, Poliovirus Types 1, 2, and 3 are each grown in separate cultures of MRC-5 cells, a line of human diploid cells obtained from the normal lung tissue of a 14-week-old male fetus. The cells are grown in CMRL 1969 medium with supplemented calf serum. After filtration and clarification, the viral suspensions are concentrated by ultrafiltration then purified by liquid chromatography and inactivated with formaldehyde. The monovalents concentrates are then combined to produce the trivalent poliovirus concentrate.
The adsorbed diphtheria, tetanus and acellular pertussis antigens are mixed with the aluminum phosphate adjuvant, 2-phenoxyethanol and water for injection. The trivalent poliovirus concentrate is then added and the DTaP-polio component is diluted to its final concentration. There is no preservative in the DTaP-polio component.
Polyribosyl-ribitol-phosphate (PRP) is made from the Haemophilus influenzae type b strain 1482 grown in a semi-synthetic medium. The tetanus toxin has been taken from the Harvard strain of Clostridium tetani, purified with ammonium sulfate, rendered inactive by formalin, and grown in a modified Mueller and Miller medium, a culture medium containing raw materials made from milk. The toxoid is sterilized prior to being conjugated. ActHIB does not contain a preservative.
VAXELIS is manufactured in partnership by Sanofi Pasteur and Merck and is indicated for vaccination against diphtheria, tetanus, pertussis, poliomyelitis, Haemophilus influenzae type b, and Hepatitis B in children ages six weeks through four years of age (prior to the fifth birthday). It is injected into the muscle in a 3-dose schedule and recommended to be administered at 2, 4, and 6 months. Specifically, according to the manufacturer’s product insert, each 0.5 mL dose of VAXELIS is formulated to contain 15 Lf diphtheria toxoid, 5 Lf tetanus toxoid, acellular pertussis antigens, 20 mcg detoxified pertussis toxin (PT), 20 mcg filamentous hemagglutinin (FHA), 3 mcg pertactin (PRN), 5 mcg fimbriae types 2 and 3 (FIM), inactivated polioviruses (29 D-antigen units (DU) Type 1 Mahoney, 7 DU Type 2 MEF-1, 26 DU Type 3 Saukett, 3 mcg polyribosylribitol phosphate (PRP) of H. influenzae type b bound to 50 mcg of the outer membrane protein complex (OMPC) of Neisseria meningitidis serogroup B, and 10 mcg hepatitis B surface antigen (HBsAg). Each 0.5 mL dose of VAXLEIS contains 319 mcg of aluminum salts as an adjuvant.
Additional ingredients in each 0.5ml dose of VAXELIS includes 319 mcg of aluminum salts as the adjuvant, <0.0056 percent polysorbate 80, less than or equal to 14 mcg residual formaldehyde, less than or equal to 50 ng residual glutaraldehyde, less than or equal to 50 ng residual residual bovine serum albumin, less than 25 ng of polymyxin B sulfate, less than 5ng of neomycin, less than 200ng of streptomycin sulfate, less than or equal to 0.1ng yeast protein, and less than or equal to 0.125 ng ammonium thiocyanate.
The Cornyebacterium diphtheria is grown in modified Mueller’s growth medium, purified by ammonium sulfate fractionation and the diphtheria toxin is detoxified with formaldehyde and diafiltered. Clostridium tetani is grown in modified Mueller-Miller casamino acid medium without beef heart infusion and the tetanus toxin is detoxified with formaldehyde then purified by ammonium sulfate fractionation and diafiltration. The tetanus and diphtheria toxoids are each adsorbed onto aluminum phosphate. The acellular pertussis antigens are produced from Bordetella pertussis cultures grown in Stainer-Scholte medium, modified by the addition of casamino acids and dimethyl-beta-cyclodextrin. PT, FHA, and PRN and are isolated individually from the culture medium. FIM are removed and copurified from the bacterial cells. The pertussis antigens are purified by sequential filtration, ultrafiltration, salt precipitation and chromoatography. PT is detoxified with glutaraldehyde, FHA is treated with formaldhyde and the residual aldehydes are removed by ultrafiltration. The antigens are adsorbed individually onto aluminum phosphate.
Poliovirus Types 1, 2, and 3 are each grown separately in VERO cells and the viral products are then concentrated and purified before becoming inactivated by formaldehyde. Each poliovirus serotype is then mixed to form the trivalent poliovirus concentrate.
The hepatitis B virus surface antigen (HBsAg) is collected and purified from fermentation cultures of a recombinant strain of the yeast Saccharomyces cerevisiae containing the gene for the adw subtype of HBsAg. This fermentation process involves growth of Saccharomyces cerevisiae on a complex fermentation medium which consists of an extract of yeast, soy peptone, dextrose, amino acids and mineral salts. The HBsAg protein is released from the yeast cells by cell disruption and purified through several methods that include hydrophobic and ion chromatography, and diafiltration. This purified protein is treated in phosphate buffer with formaldehyde and then coprecipitated with potassium aluminum sulfate and amorphous aluminum hydroxyphosphate sulfate to form the vaccine adjuvant.
The purified polyribosylribitol phosphate (PRP) of H. influenzae type b (Haemophilus b, Ross strain) is covalently bound to an outer membrane protein complex (OMPC) of the B11 strain of Neisseria meningitides serogroup B. H. influenzae type b is grown in a fermentation medium which includes hemin chloride, soy peptone, an extract of yeast, nicotinamide adenine dinucleotide, dextrose, and mineral salts. The PRP is purified by procedures which include phenol extraction, ethanol fractionation, enzyme digestion, and diafiltration. N. meningitidis serogroup B is grown on a complex fermentation medium which consists an extract of yeast, amino acids and mineral salts. The OMPC is purified by, sterile filtration, ultracentrifugation, diafiltration, and detergent extraction. PRP is conjugated to OMPC by chemical coupling and then adsorbed onto an amorphous aluminum hydroxyphosphate sulfate adjuvant.
The adsorbed diphtheria, tetanus, and acellular pertussis antigens are mixed with aluminum phosphate, as an adjuvant, and water for injection into an intermediate concentrate. The individual hepatitis B virus surface antigen (HBsAg) and PRP-OMPC adjuvanted products are then added and followed by the trivalent poliovirus concentrate, to produce VAXELIS.
VAXELIS does not contain a preservative and the vaccine’s vial stopper does not contain natural rubber latex.
The CDC has approved Hib vaccine for use in children at 2, 4, 6 and 12-15 months of age and also recommends Hib vaccine for individuals over the age of five years who lack a functioning spleen, including persons with sickle cell anemia, as well as to individuals who will be having their spleen removed as an elective surgery. Additionally, hematopoietic stem cell transplant recipients are also recommended to receive three doses of Hib vaccine four weeks apart beginning at least six months following transplant. It is important to note that while the CDC has recommended the use of Hib vaccines to persons over the age of five with the aforementioned medical conditions, no Hib vaccines are FDA approved for use in persons age five and older.
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
What is the history of Hib vaccine in America?

In the 1970’s, scientists began research on a vaccine using a purified polysaccharide, polyribosylribitol phosphate (PRP) for the prevention Haemophilus influenzae type b. This polysaccharide vaccine only induced protective antibody levels in children older than 18 to 24 months old and revaccination did not induce a booster effect at any age. As a result, researchers reported that if they were going to achieve immunoprophylactic control of meningitis caused by Hib, they were going to have to come up with a more effective vaccine. Despite the limited effectiveness of Hib polysaccharide vaccines, these vaccines received FDA approval for use in 1985. The CDC reported the vaccines to be effective in children older than two years and in adults, however, they acknowledged their ineffectiveness in children under the age of 18 months. In children between the ages of 18 and 23 months, the immune response following vaccination was found to be lower than in persons aged two years and older.
When the FDA approved the first Hib polysaccharide vaccines in 1985, the duration of vaccine acquired immunity was not known but estimated to be at only 1.5 to 3.5 years. Children between the ages of six months and one year of age were considered to be the most susceptible to Haemophilus influenzae invasive disease and only 35 to 40 percent of Hib cases occurred in children 18 months of age and older. In 1985, the CDC recommended that all children receive a single dose of polysaccharide vaccine at 24 months, but stated that vaccination could begin at 18 months of age if a child was considered at a high risk for developing Hib invasive disease. Children attending daycare, children with immunosuppression related to cancer, and children with asplenia were reported to be at a higher risk for Hib invasive disease. The CDC, however, cautioned that while the vaccine could be administered in children as young as 18 months of age, it may not effective in children between the ages of 18 and 24 months. Three Hib polysaccharide vaccines received approval in 1985: b Capsa 1 manufactured by Praxis; HibImmune, manufactured by Lederle; and HibVAX, manufactured by Connaught.
Studies on the effectiveness of polysaccharide Hib vaccines for the prevention of invasive H. influenzae type b disease varied significantly with vaccine effectiveness reported to be between 88 and -69 percent (with the negative efficacy indicating that vaccination increased the likelihood of Hib infection). Additional studies also noted an increased risk for the development of invasive Hib disease within seven days following the administration of the polysaccharide Hib vaccine. In the 1994 review of vaccine adverse events completed by the Institute of Medicine (IOM), a causal association was favored by the committee between an increased risk of early onset H. influenzae disease in children older than 18 months who received an unconjugated PRP vaccine as their first Hib vaccine. All Hib polysaccharide vaccines were discontinued in 1989, four years following their initial FDA approval.
After researchers discovered that a conjugation process resulted in a better immune response, the first conjugated Hib vaccine, ProHIBIT, was introduced in the U.S. in December 1987. This first conjugated Hib vaccine linked the Haemophilus b capsular polysaccharide to a diphtheria toxoid, and in January 1988, the CDC’s Advisory Committee on Immunization Practices (ACIP) recommended routine use of the vaccine for all children beginning at 18 months of age. At the time of this recommendation, however, ACIP acknowledged that “the efficacy of conjugate vaccine in children 18 months of age or older has not been determined in field trials.” The approval was based on studies that compared Hib antibody levels in children who received the newly approved conjugated Hib vaccine, against those who were administered the previously approved Hib polysaccharide vaccine. Study results suggested that the conjugated Hib vaccine would offer greater protection than Hib polysaccharide vaccines.
In December of 1988, HibTITER, a second Hib conjugated vaccine, received FDA approval for use in children 18 months of age and older. However, prior to the FDA approval, Praxis, the manufacturer of HibTITER, was found to have engaged in misleading promotional activities. Praxis had claimed HibTITER to be superior in quality and purity, and would offer a greater immune response than the currently available Hib vaccines and the statements resulted in four separate warning letters from the FDA. As well, following FDA approval of HibTITER for use in children 18 months of age and older, Praxis was found to be in violation of the Federal Food, Drug, and Cosmetic Act (FD&C Act) on five separate occasions. In particular, Praxis had released a draft scientific article written by five of the company’s scientists in December of 1988 reporting on the use of the vaccine in young infants, despite the fact that the vaccine was not yet approved for use in children under the age of 18 months. HibTITER was not FDA approved for use in infants aged 2 months and older until October of 1990.
In December of 1989, PedvaxHIB, a conjugated Hib vaccine bound to a meningococcal protein (PRP-OMP) manufactured by Merck, Sharpe, and Dohme, received FDA approval for use in children 18 months of age and older. The FDA also gave approval for the vaccine to be used in children as young as 15 months of age if it were determined that the child would not return at 18 months of age to be vaccinated. In April of 1990, ACIP issued a recommendation for the routine use of Hib vaccination beginning at 15 months of age.
In October of 1990, the FDA expanded the use of HibTITER in children under the age of 18 months by approving the vaccine for use in infants beginning at two months of age. HibTITER was recommended to be administered as a 3 dose primary vaccine series, at 2, 4, and 6 months of age. The CDC also recommended that previously unvaccinated infants between 7 and 11 months of age receive two doses of the vaccine, two months apart. Previously unvaccinated children between 12 and 14 months of age were recommended to receive a single dose, with a booster dose after 15 months and unvaccinated children between 15 and 60 months were recommended to receive a single dose of the vaccine.
Two months later, in December of 1990, the FDA expanded the use of Merck’s PedvaxHIB, for use in infants beginning at two months of age. PedvaxHIB was recommended to be administrated as a 2-dose primary series at 2 and 4 months, with a booster dose at 12 months. Two year later, in November of 1992, Merck reported that 16 PedvaxHIB lots, or 366,000 doses “may have lower than expected immunogenicity.” Merck stated that it would be contacting physicians who received doses of the vaccines from these lots to suggest that certain vaccine recipients receive an additional Hib dose.
On March 30, 1993, the FDA approved two more Hib conjugated vaccines for use in infants as young as two months of age. ActHIB, a polyribosylribitol phosphate-tetanus toxoid conjugate Haemophilus b vaccine, (PRP-T), manufactured by Pasteur Merieux Serum et Vaccins (now Sanofi Pasteur) and distributed in the U.S. by Connaught Laboratories and TETRAMUNE, a combined diphtheria and tetanus toxoid, whole cell pertussis and Haemophilus b conjugate vaccine, made available by Lederle-Praxis Biologicals. TETRAMUNE combined the previously licensed DTP vaccine, TRI-IMMUNOL, with HibTITER, a Haemophilus b conjugate vaccine.
In September 1993, ACIP issued recommendations for the use of both the available Haemophilus b conjugate vaccine as well as the combined diphtheria, tetanus, whole cell pertussis, and Haemophilus b conjugate vaccine. At the time of this recommendations, there were five FDA approved Hib containing vaccines, with four vaccines approved for use in children beginning at two months of age (HibTITER, PedvaxHIB, ActHIB, and the combined DTP-Hib vaccine, TETRAMUNE). The fifth vaccine, ProHIBIT, was approved for use only as a booster dose following completion of a primary two or three dose vaccine series, or as single dose in children between the ages of 15 and 59 months.
On September 27, 1996, the first combined diphtheria, tetanus, acellular pertussis, and Haemophilus b vaccine, TriHIBit, received FDA approval for use as the fourth dose of the vaccine series to be administered to children between the ages of 15 and 18 months. TriHIBit combined Tripedia, a newly approved diphtheria and tetanus toxoid and acellular pertussis vaccine, with the Hib conjugated vaccine, ActHIB. In late July of 1996, Tripedia became the first DTaP vaccine approved by the FDA for use in infants beginning at two months of age, and was recommended for use by ACIP in lieu of the highly reactive whole cell DTP vaccine. Prior to this July 1996 recommendation, the DTaP vaccine was approved only for use in children who had previously received three doses of DTP, at 2, 4, and 6 months of age. However, as Tripedia was approved for use in infants as young as two months of age, confusion resulted in regards to the use of TriHIBIT. TriHIBIT was only FDA approved for use as the fourth Hib dose, to be administered between 15 and 18 months, however, health care providers were found to be using TriHIBIT in children as young as two months. As a result, the CDC was required to issue a warning in September of 1988 in regards to the unlicensed use of TriHIBIT.
In October 1996, Merck’s Comvax, a vaccine combining PedvaxHIB with RECOMBIVAX HB, a previously approved recombinant hepatitis B vaccine, received FDA approval for use in infants and children, and was recommended by the CDC to be administered at 2, 4, and 12-15 months of age. Infants receiving a birth dose of Hepatitis B vaccine, as recommended by ACIP, would receive an additional fourth dose of Hepatitis B vaccine between 12 and 15 months of age, if administered the three recommended Comvax doses. Merck discontinued Comvax in 2014.
On December 13, 2007, Merck announced a voluntary recall of several vaccine lots of both PedvaxHIB (Hib conjugate vaccine) and Comvax (Hib conjugate/Hepatitis B vaccine) related to a manufacturing issue. Merck reported that it could not guarantee the sterility of the equipment used to manufacture certain lots of the vaccines and as a result, issued the recall. The recall and anticipated Hib vaccine shortage prompted the CDC to recommend that healthcare providers defer the booster dose of Hib vaccine typically administered between 12 and 15 months of age in children not considered to be at high risk for invasive Hib disease. It was late June 2009 before the CDC recommended that the booster dose of Hib vaccine be reinstated for all children.
In response to the shortage of available Hib vaccines resulting from Merck’s vaccine sterility issues, the FDA allowed GlaxoSmithKline HIBERIX, an additional Haemophilus b conjugate vaccine, to receive approval under the Accelerated Approval Regulations. The Accelerated Approval process allows drugs and vaccines targeting serious conditions that fill an unmet medical need to be approved based on a surrogate endpoint. A surrogate endpoint is a marker such as radiographic image, a physical sign, a laboratory measurement, or other tool of measurement that is thought to predict clinical benefit of the product, but is not actually a measure of clinical benefit. By using this surrogate endpoint, the FDA can accelerate approval of drugs and vaccines. HIBERIX initially received FDA approval in August of 2009 for use in children between the ages of 15 months and four years of age, however, in January of 2016, the FDA expanded the use of HIBERIX, allowing the vaccine to be used as the primary 3-dose Hib series in children as young as six weeks of age.
In June of 2008, Pentacel, a combination diphtheria and tetanus toxoid and acellular pertussis (DTaP), inactivated poliomyelitis, and Haemophilus influenzae type b conjugate vaccine manufactured by Sanofi Pasteur, was FDA approved for use as a four-dose series at 2, 4, 6, and 12-15 months. Pentacel combined ActHIB Hib vaccine with the polio vaccine, Poliovax, and the DTaP vaccine Daptacel, however, Pentacel contained twice as much detoxified PT and four times as much FHA as Daptacel.
On June 14, 2012, MenHibrix, a Meningococcal Groups C and Y and Haemophilus b Tetanus Toxoid Conjugate Vaccine manufactured by GlaxoSmithKline received FDA approval for use in infants and children between six weeks and 18 months of age. At the October 2012 ACIP meeting, MenHibrix was recommended exclusively for use in infants and children determined to be at higher risk for meningococcal disease. Included in this recommendation were infants found to have anatomical or functional asplenia, including sickle cell disease, and those with persistent complement pathway deficiencies. MenHibrix was also approved for use in communities dealing with outbreaks of meningococcal group C and Y, but not recommended for routine use due to the low number of cases of group C and Y meningococcal disease in the United States. In October 2016, citing low demand for the product, GlaxoSmithKline announced the discontinuation of MenHibrix vaccine in the United States.
In December of 2016, a small Pennsylvania newspaper reported that between 2013 and 2015, Sanofi Pasteur had permitted two glass contaminated ActHIB vaccine lots to be administered to infants and young children. The Morning Call pieced together information acquired through the Freedom of Information Act (FOIA) and reported that Sanofi Pasteur, who became aware of the glass contaminated lots on April 2, 2013, had declined to issue a recall. The two contaminated vaccine lots had already been shipped and would remain available for use until their expiration dates of September 5 and 6, 2014.
Sanofi Pasteur placed blame on the vaccine’s vial manufacturer and promptly changed suppliers, however, the company waited over two months before notifying the FDA. Despite noting fifteen shortcomings in regards to Sanofi’s response to the glass contamination, the FDA also declined to issue a recall of the contaminated vaccines. By November of 2014, the FDA had completed its investigation and stated that Sanofi had “acted responsibly” by correcting the problem. In addition to the 2013 contamination, Sanofi Pasteur notified the FDA on two separate occasions in January 2015 and again in March of 2015, of other contaminated ActHIB lots. In January of 2015, Sanofi reported that a previously distributed lot that had expired in March of 2014, had contained stainless steel particulates. On March 30th, 2015, the FDA was again notified of glass contamination involving another lot of ActHIB vaccine, with an expiration date of August 5, 2014. While no adverse events have been reported to be directly associated with the administration of the glass contaminates, the FDA has warned that blood clots and other serious vascular events can occur when glass is administered subcutaneously.
There are five Haemophilus influenzae type b (Hib) vaccines available for use in the United States: ActHIB; HIBERIX; PedvaxHIB; Pentacel (Hib vaccine combined with diphtheria and tetanus toxoids, acellular pertussis adsorbed, and inactivated poliovirus); and VAXELIS, a 6 in 1 (hexavalent) vaccine containing Haemophilus influenzae type b conjugate vaccine in combination with diphtheria and tetanus toxoid and acellular pertussis (DTaP), inactivated poliomyelis (IPV), and recombinant hepatitis B vaccine.
The CDC recommends that all infants and young children receive Hib vaccine at 2, 4, and 6 months of age with an additional booster dose between 12 and 15 months of age. Hib vaccine is also recommended by the CDC for use in older children, adolescents and adults with certain medical conditions, however, no Hib vaccines are currently FDA approved for use in persons over five years of age.
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
How effective is Hib vaccine?
.jpg.aspx?width=152&height=205)
According to the CDC, 95 percent of infants vaccinated with two or three doses of Hib conjugate vaccines will develop antibodies thought to be indicative of protection against Haemophilus influenzae type b invasive disease, however, the duration of vaccine acquired immunity from Hib vaccines is unknown.
The immunogenicity of Hib vaccine varies with severity of immunocompromised and stage of infection in persons with HIV infection. The CDC reports Hib vaccines to be effective in persons considered at higher risk for invasive disease, including persons with HIV infection, asplenia, leukemia, and sickle cell disease, however, no efficacy studies have ever been completed to determine the actual effectiveness of the use of Hib vaccines in these high-risk populations.
According to the manufacturer’s package insert, ActHIB induces antibodies in 90 percent of infants after the primary series and 98 percent of infants after a booster dose. However, Native Americans, a population noted to be at greater risk of Hib invasive disease, have a lower immune response to Hib conjugate vaccines. Sanofi Pasteur reports that following a full three doses of the vaccine administered between six weeks and six months of age, only 75 percent of Native American infants had acceptable antibody levels. In children with sickle cell anemia, only 89 percent of children had acceptable antibodies after two doses of ActHIB. If ActHIB is administered to immunosuppressed individuals, including those receiving immunosuppressive therapy, expected antibody responses may not be obtained. This population includes patients with asymptomatic or symptomatic HIV-infection, severe combined immunodeficiency, hypogammaglobulinemia or agammaglobulinemia; altered immune status due to diseases such as leukemia, lymphoma, or generalized malignancy, or an immune system compromised by treatment with corticosteroids, alkylating drugs, antimetabolites or radiation.
According to the manufacturer’s package insert for HIBERIX, based on a clinical efficacy study with unconjugated Haemophilus b polysaccharide vaccine and data from passive antibody studies, an anti-PRP concentration of 0.15 mcg/mL is considered to be the minimal protective level against Hib invasive disease. Data collected from an efficacy study of unconjugated Haemophilus b polysaccharide vaccine indicates that an anti-PRP concentration of ≥1.0 mcg/mL is predictive of protection against invasive Hib disease through at least a one-year period. In vaccine efficacy studies, these two particular antibody levels have been used to evaluate the effectiveness of Haemophilus b conjugate vaccines, including HIBERIX. One month following the completion of the three dose Hib primary vaccine series, 96.6 percent of infants were found to have passive antibodies equal to or greater than 0.15 mcg/mL while only 81.2 percent were found to have levels greater than or equal to 1.0 mcg/mL. One month following a booster dose of HIBERIX administered between 15 and 18 months of age, 100 percent of children were found to have passive antibodies equal to or greater than 0.15mcg/mL and 99.1 percent were found to have levels greater than or equal to 1.0 mcg/mL. The safety and effectiveness of HIBERIX in immunosuppressed children, including children receiving immunosuppressive therapy, has not been evaluated and if administered to this population, the expected immune response may not be obtained. Immunosuppressive therapies that may reduce immune response to HIBERIX include irradiation, antimetabolites, alkylating agents, cytotoxic drugs and corticosteroids used in greater than physiologic doses.
According to the manufacturer’s package insert, the protective efficacy of PedvaxHIB measured during clinical trials of high-risk populations was estimated to be 93 to 100 percent, depending on the age of the child. For the maintenance of vaccine induced antibody levels, a booster dose of PedvaxHIB is required in infants who complete the primary two-dose regimen prior to 12 months of age.
According to the manufacturer’s package insert, the protective efficacy of the pentavalent vaccine Pentacel may not extend to all individuals. If Pentacel is administered to immunocompromised persons, including those receiving immunosuppressive therapy, the expected immune response may not be obtained. Immunosuppressive therapies, including irradiation, antimetabolities, alkylating agents, cytotoxic drugs and corticosteroids used in greater than physiologic doses may also reduce the immune response to Pentacel. Neither the safety nor the effectiveness of Pentacel in infants less than six weeks old or in children ages five to 16 years old have been established.
In clinical studies with Pentacel, efficacy was measured by antibody responses to the individual five disease components contained in the vaccine. Hib antibodies were found to be between 90 and 98.2 percent, depending on the study.
In VAXELIS pre-licensing clinical trials, efficacy was measured by examining antibody responses to the individual six disease components found in the vaccine. Immune responses were evaluated by the manufacturers one month following completion of the three dose VAXELIS vaccine series. For HIB, 97.3 percent of clinical trial participants were found to have anti-PRP levels greater than or equal to 0.15 ug/mL while 85 percent were noted to have anti-PRP levels greater than or equal to 1.0 ug/mL. Anti-PRP levels greater than or equal to 1.0 ug/mL measured three weeks following Hib vaccination are considered to be predictive of protection for one year.
Data on the safety and effectiveness of using VAXELIS following the use of one or two doses of DTaP, IPV, HIB, or hepatitis B vaccine manufactured by another vaccine maker is not available. The protective efficacy of the hexavalent vaccine VAXELIS may not extend to all individuals. If VAXELIS is administered to immunocompromised persons, including those receiving immunosuppressive therapy, the expected immune response may not be obtained.
While Hib vaccines have been reported to be highly effective by vaccine manufacturers, independent studies have noted that vaccine failure can occur, resulting in invasive Hib disease. Additionally, several studies have found an increase in non-b type invasive H. influenzae infections since Hib vaccines were first introduced. H. influenzae type e and type f have increased in the United States while Northern Canada and Alaska have noted a significant increase in H. influenzae type a invasive disease. An increase in H. influenzae type a was also noted among children in Utah. Brazil experienced a substantial increase in H. influenzae type a meningitis following the introduction of vaccines targeting H. influenzae type b. In Ontario Canada, following the introduction of Hib vaccines, nontypeable and type f H. influenzae invasive disease have reportedly replaced H. influenzae type b in children under the age of five. Further, since the introduction of both Hib conjugate vaccines and pneumococcal conjugate vaccines, nontypeable H. influenzae has emerged as a serious health threat. While nontypeable H. influenzae is most noted to be associated with otitis media and sinusitis in children as well as acute exacerbation of chronic obstructive pulmonary disease (COPD) in adults, it can also result in invasive disease.
Hib vaccines can offer protection from invasive H. influenzae type b infections, however, they are not protective against invasive disease caused by non-b type or nontypeable H. influenzae. Moreover, the long-term effectiveness of Hib vaccines is not known at this time.
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
Can Hib vaccine cause injury & death?

According to the CDC, mild side effects such as redness, warmth, or swelling where the shot was given have been reported in connection with administration of Hib vaccines. Fever has also been reported following vaccination. Other adverse events that may occur include dizziness, fainting, allergic reaction, other serious injury and death.
In pre-licensing clinical trials, the severity of adverse reactions varied depended on which vaccine was given, as well as the additional vaccines administered simultaneously. Some of the events reported by the manufacturers included:
ActHIB — tenderness, erythema, swelling, induration, fever, irritability, drowsiness, anorexia, unusual or persistent crying, vomiting, and seizure with apnea. Reported side effects post marketing have included convulsions, anaphylaxis, peripheral edema, extensive limb swelling, pruritus, and rash. Initial pre-licensing clinical safety studies of ActHIB compared the vaccine against other vaccines such as hepatitis B, while other studies involved ActHIB to be administered in addition to multiple vaccines including the DTP vaccine. Additional clinical studies on ActHIB involved the solicitation of adverse events when the vaccine was administered along with DTaP, IPV (polio), PCV7, and hepatitis B vaccines. No clinical studies involved a comparison of ActHIB against a true placebo.
HIBERIX —redness, pain and swelling at injection site, fever, fussiness, irritability, loss of appetite, restlessness, sleepiness, diarrhea, vomiting, seizure, bilateral pneumonia; Reported side effects post marketing have included extensive swelling of the vaccinated limb, anaphylactic reactions, angioedema, convulsions, hypotonic-hyporesponsive episode, syncope, apnea, rash, urticaria, somnolence. Pre-licensing clinical trials of HIBERIX did not involve the use of a true placebo and most trials involved the testing of HIBERIX against another licensed Hib vaccine in combination with multiple additional vaccines. For example, one pre-licensing clinical safety study compared HIBERIX to another U.S. licensed Hib vaccine administered along with PEDIARIX vaccine (combination DTaP, inactivated polio, and hepatitis B vaccine). Study participants who received HIBERIX or another U.S. licensed Hib vaccine also received a dose of PEDIARIX and a dose of PCV13 (13-valent pneumococcal vaccine) at all three doses AND a dose of ROTARIX live oral rotavirus vaccine at dose 1 and 2. Study participants receiving PEDIARIX also received a dose of PCV13 and a dose of ENGERIX-B (Hepatitis B vaccine) when indicated, dependent on whether a dose of hepatitis B vaccine was administered at birth.
PedvaxHIB —irritability, sleepiness, injection site pain/soreness, injection site swelling/induration, injection site erythema, prolonged crying (more than 4 hours), unusual high-pitched crying, vomiting, diarrhea, pain, crying, otitis media, rash, upper respiratory infection, seizures, tracheitis, thrombocytopenia, urticaria; potential adverse events may also include early onset of Hib disease and Guillain-Barre syndrome (GBS); Reported side effects post marketing have included lymphadenopathy, febrile seizures, angioedema, and injection site abscess. Pre-licensing clinical trials of liquid PedvaxHIB compared the vaccine to lyophilized PedvaxHIB with most children in each study group receiving the DTP and oral polio vaccine in addition to PedvaxHIB. No pre-licensing clinical trials involved the comparison of PedvaxHIB against a true placebo.
Pentacel — irritability, fussiness, inconsolable crying, injection site redness, swelling, tenderness, increase in arm circumference (dose 4), fever, lethargy, hypotonic hyporesponsive episodes (HHE), seizures, febrile seizures, bronchiolitis, dehydration, pneumonia, gastroenteritis, asthma, pneumonia, encephalopathy, and four deaths attributed to asphyxia due to suffocation, head trauma, sudden infant death syndrome (SIDS), and neuroblastoma. Reported side effects post marketing have included cyanosis, vomiting, diarrhea, extensive swelling of injected limb including swelling that involved adjacent joints, invasive Hib disease (classified as vaccine failure), rash, urticarial, meningitis, rhinitis, viral infection, decreased appetite, somnolence, hypotonic hyporesponsive episodes, depressed level of consciousness, screaming, apnea, cough, erythema, skin discoloration, and pallor. In pre-licensing clinical safety trials of Pentacel, there were no true placebo studies and most clinical trials compared the product against multiple vaccines including DTaP (diphtheria, tetanus, and acellular pertussis vaccine), polio vaccine, and ActHIB (Hib conjugated vaccine). In addition to the administration of Pentacel or the control vaccine(s), study participants also received PCV7 (7-valent pneumococcal vaccine, hepatitis B vaccine, and in some trials, measles, mumps, rubella (MMR) and varicella vaccines were also administered. Additionally, one pre-licensing clinical safety studies did not have a control group and involved the evaluation of adverse events reported following the fourth dose of Pentacel.
Pentacel was first licensed in Canada in May of 1997, and data reported from Canada was evaluated by the FDA as part of the licensing process. In Canada, between May 1, 1997 and April 30, 2006, there were 245 medically confirmed adverse events reported to the manufacturer, with 237 adverse events reports submitted by health care authorities and providers and eight reports pulled from literature. There were also 43 adverse events reported from health care consumers. Adverse events included: vomiting; diarrhea; cyanosis; eye rolling; injection site reactions including pain, inflammation, mass, and abscess; fever, irritability; edema, including peripheral edema; decreased vaccine response and vaccine failure; sudden infant death syndrome; sudden death; viral infection; rhinitis; meningitis; decreased appetite; seizures; hypotonic-hyporesponsive episode; somnolence; hypotonia; lethargy; encephalopathy; depressed level of consciousness; rash, including maculo-papular; skin discoloration; urticaria; and pallor. Fourteen deaths were reported following the administration of Pentacel and causes included Sudden Infant Death Syndrome (5 cases), unknown causes (4 cases), invasive Hib disease (2 cases), sepsis (1 case), convulsions (1 case), congenital anomaly (1 case).
In addition to the deaths that occurred during the Pentacel clinical trials, deaths following the administration of other pentavalent vaccines have also been reported. In a March 2012 open letter to Dr. Margaret Chan, then director general of the World Health Organization, the letter’s authors called attention to the deaths connected with the pentavalent (DPT + Hib + Hepatitis B) vaccine in India, Sri Lanka, Bhutan, and Pakistan and noted the cause of the problem to be unrelated to the brand, manufacturer or lot of the vaccine, while stating that:
“It appears to be a form of ‘hypersensitivity reaction’ as described in the post mortem report on one of the children in Kerala. The vaccine can be administered to many patients without problems and there is no available method at present to predict which infant will react adversely.”
Several studies on a Hib containing pentavalent vaccine used in South Asia and India have reported an elevated risk of death following vaccination, with several physicians publicly rejecting the use of the pentavalent vaccine.
In a pediatric safety and use review of Pentacel presented in March of 2010, Dr. Jane Woo with the FDA discussed reported adverse reactions related to the vaccine following the June 2008 FDA approval. At the meeting, Dr. Woo reported that 775 adverse reactions, 170 of which were considered serious including 26 deaths, had been reported to VAERS in connection with Pentacel between June 20, 2008 (when Pentacel was licensed) and October 31, 2009. Deaths were attributed to SIDS (almost half of the reported cases), congenital/genetic conditions, respiratory infections, positional asphyxia, anoxic encephalopathy, cardiac arrest of undetermined etiology, dilated and hypertrophic cardiomyopathy, two deaths of undetermined cause, one death with no records obtainable, and two deaths with information pending. Dr. Woo stated that the number of cases of SIDS were not concerning and went on to quote the Institute of Medicine (IOM), which had previously concluded that evidence favors rejection of a causal relationship between exposure to multiple vaccines and SIDS.
VAXELIS – injection site pain, swelling, and redness, crying, fever, irritability, decreased appetite, vomiting, somnolence, and death. At this time, post-marketing data on serious adverse events are limited to those events considered to have a causal link to the vaccines containing the antigens of VAXELIS. These include anaphylaxis, hypersensitivity, seizures, including febrile seizures, and excessive swelling of the injected limb. 6 in 1 (hexavalent) vaccines have been in use outside of the United States for several years and numerous studies have linked their use to an increase in infant deaths. In the two U.S. pre-licensing clinical trials, six deaths were reported in infants who received VAXELIS and included sepsis, asphyxia, hydrocephalus, unknown cause, and two cases of sudden infant death syndrome. The number of deaths that occurred during the VAXELIS pre-licensing clinical trials outside of the United States was not provided as part of the vaccine product insert. Pre-licensing clinical trials of VAXELIS compared infants who received VAXELIS concomitantly with RotaTeq (rotavirus vaccine) and Prevnar 13 (13-valent pneumococcal conjugate vaccine) against infants who received Pentacel (DTaP-IPV-HIB), and RECOMBIVAX-HB (hepatitis B, recombinant vaccine) concomitantly with RotaTeq and Prevnar 13. The safety and effectiveness of VAXELIS was evaluated in six clinical trials involving only 5,251 infants between the ages of 43 and 99 days of age at the time of enrollment. Only two clinical trials took place in the United States and involved 3,380 infants between the ages of 46 and 98 days. Information on solicited adverse events included injection site pain, redness, and swelling, fever, irritability, decreased appetite, somnolence, vomiting and crying were recorded by parents for only five days following vaccination. Sixty-eight (2 percent) infants who received VAXELIS were reported to have experienced a serious adverse event within 30 days of vaccination, however, only four of these serious adverse events were attributed to VAXELIS. Three infants experienced serious fever and one infant had a life-threatening event that included vomiting followed by lethargy and pallor. The VAXELIS product insert does not provide any further information on the serious adverse events reported post vaccine administration that were considered by the vaccine manufacturer to be unrelated to the administration of VAXELIS. While VAXELIS is FDA approved for use in infants and children between the ages of six weeks and four years of age, the safety of VAXELIS was only evaluated in infants and children between six weeks and 15 months and the effectiveness of VAXELIS was only evaluated in infants between six weeks and six months of age. Pre-licensing clinical trials did not examine the effectiveness of VAXELIS in infants and children between six months and four years of age or the safety of VAXELIS for use in children between 15 months and four years of age. The FDA granted approval of the vaccine for use in this older population based on pre-licensing clinical trial data involving only younger children. Currently, there are no studies to support the safety of VAXELIS for use in children between the ages of 15 months and four years of age.
Using the MedAlerts search engine, as of March 29, 2024, there have been 93,508 reports of Hib vaccine reactions, hospitalizations, injuries and deaths following Hib vaccinations made to the federal Vaccine Adverse Events Reporting System (VAERS), including 2,927 related deaths, 19,094 hospitalizations, and 1,826 related disabilities. Approximately 85 percent of HIB vaccine-related adverse events occurred in children under three years of age. Of these Hib-vaccine related deaths reported to VAERS,nearly 92 percent of the deaths occurred in children under three years of age. Of these reported deaths, 2,177 occurred in infants under the age of 6 months.
Even though the National Childhood Vaccine Injury Act of 1986 legally required pediatricians and other vaccine providers to report serious health problems following vaccination to federal health agencies (VAERS), many doctors and other medical workers giving vaccines to children and adults fail to report vaccine-related health problem to VAERS. There is evidence that only between one and 10 percent of serious health problems that occur after use of prescription drugs or vaccines in the U.S. are ever reported to federal health officials, who are responsible for regulating the safety of drugs and vaccines and issue national vaccine policy recommendations.
As of April 1, 2024, there had been 179 claims filed in the federal Vaccine Injury Compensation Program (VICP) for injuries and deaths following HIB vaccination, including 34 deaths and 145 serious injuries. Of that number, the U.S. Court of Claims administering the VICP has compensated 61 children and adults who have filed for Hib vaccine injuries.
In the comprehensive report evaluating scientific evidence, Adverse Events Associated with Childhood Vaccines: Evidence Bearing on Causality, published in 1994 by the Institute of Medicine (IOM), reported vaccine adverse events following administration of Haemophilus influenzae vaccines were evaluated by a physician committee. These adverse events included Guillain-Barre Syndrome, transverse myelitis, thrombocytopenia, early susceptibility to H. influenzae type b, anaphylaxis, and death. In most cases, after evaluating the available literature, the IOM was unable to accept or reject a causal relation between Hib vaccines and the reported side effect due to a lack of evidence. The committee, however, favored a causal association between unconjugated PRP vaccine (unconjugated PRP vaccines are no longer approved for use in the U.S.) and the increased risk of early onset H. influenzae disease in children older than 18 months who received an unconjugated PRP vaccine as their first Hib vaccine. The committee also favored rejection of an association between early onset Hib disease and conjugated Hib vaccines (conjugated Hib vaccines are the only FDA approved Hib vaccines available in the U.S.) Additionally, the IOM favored rejection of a causal relation between death from early-onset Hib disease and conjugated Hib vaccines. Hib vaccines were not evaluated as part of the Institute of Medicine’s 2012 comprehensive report Adverse Effects of Vaccines: Evidence and Causality.
No Hib conjugate or Hib combination vaccines have ever been evaluated for their carcinogenic or mutagenic potential, or for impairment of fertility.
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
Who is at highest risk for complications from Hib vaccine?

There is a gap in medical knowledge in terms of doctors being able to predict who will have an adverse reaction to Haemophilus influenzae type b vaccination, and who will not.1
Persons at highest risk for complications from Hib vaccine are those who are advised not to get Hib vaccine.
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
Who Should Not Get Hib Vaccine?

According to the CDC anyone who has ever had a life-threatening allergic reaction to a previous dose of Hib vaccine should not get another dose. Children under 6 weeks old should not get this vaccine either. Also, people who are moderately or severely ill at the time the shot is scheduled should wait until they recover before getting this vaccine.
While the CDC recommends Hib vaccines for high risk populations older than the age of five which include persons without a functioning spleen, as well as hematopoietic stem cell transplant recipients, there are no Hib vaccines that are FDA approved for use in anyone five years of age and older.
According to the manufacturer’s product inserts:
- ActHIB should not be given to children with a history or hypersensitivity to a previous dose of H. influenzae type b or tetanus toxoid vaccine or any component of the vaccine. ActHIB is approved for use in infants and children two months through five years of age. Infants younger than two months of age, and children older than five should not receive ActHIB. If Guillain-Barre syndrome has occurred within six weeks of receipt of a prior vaccine containing tetanus toxoid, the decision to give ActHIB should be based on careful consideration of the possible risks and benefits of vaccination. No human or animal studies have assessed the safety of administering ActHIB during pregnancy.
- HIBERIX should not be given to anyone who has suffered a severe allergic reaction or anaphylaxis after a previous dose of any Hib or tetanus-toxoid-containing vaccine or any component of HIBERIX. HIBERIX is approved for use in infants and children six weeks through four years of age, prior to their fifth birthday. Infants younger than six weeks of age, and children five years of age and older should not receive HIBERIX. If Guillain-Barre syndrome has occurred within six weeks of receipt of a prior vaccine containing tetanus toxoid, the decision to give HIBERIX should be based on careful consideration of the possible risks and benefits of vaccination. Apnea in infants born prematurely has been associated with the administration of intramuscular injections, including HIBERIX. Administration of this vaccine should only be considered after careful assessment of the infant’s health status, along with the potential risks and benefits of vaccination. The safety and effectiveness of the HIBERIX vaccine for use in children who are immunosuppressed has not been evaluated. HIBERIX is not approved for use in pregnant or lactating women.
- PedvaxHib should not be given to anyone with a hypersensitivity to any component of the vaccine or the diluent. Persons who develop symptoms suggestive of hypersensitivity after an injection should not receive further injections of the vaccine. Use caution with children allergic to latex as the vial stopper contains dry natural latex rubber. The decision to administer or delay vaccination because of current or recent febrile illness depends on the severity of symptoms and etiology of the disease. Persons with moderate or severe febrile illness should be vaccinated after they have recovered. Persons over age six years or infants under six weeks of age should not get PedvaxHib. PedvaxHib is a Pregnancy Category C product and it is not known whether this vaccine can cause fetal harm. As a result, PedvaxHib is not recommended for use in pregnant women. This vaccine is NOT recommended for use in adult populations.
- Pentacel should not be given to anyone who has suffered a severe allergic reaction (anaphylaxis) after a previous dose of this vaccine, any ingredient of Pentacel vaccine, or any other diphtheria toxoid, tetanus toxoid, pertussis-containing vaccine, inactivated poliovirus vaccine or Hib vaccine. Pentacel should not be given to anyone who has suffered encephalopathy within seven days of a previous pertussis-containing vaccine with no other identifiable cause. Persons with a progressive neurologic disorder should not receive Pentacel until a treatment regimen has been established and the condition has stabilized. Careful consideration should be given to the benefits and risks of Pentacel before administering the vaccine to someone with a history of fever at or above 105 degrees F, a hypotonic-hyporesponsive episode, or persistent, inconsolable crying lasting more than three hours within 48 hours after a pertussis-containing vaccine, or who has suffered seizures within three days after a previous pertussis-containing vaccine. If Guillain-Barre syndrome occurred within six weeks of receipt of a prior vaccine containing tetanus toxoid, the risk for Guillain-Barre syndrome may be increased following Pentacel. Apnea in infants born prematurely has been associated with the administration of intramuscular injections, including Pentacel. Administration of this vaccine should only be considered after careful assessment of the infant’s health status, along with the potential risks and benefits of vaccination. Pentacel is a Pregnancy Category C product and it is not known whether this vaccine can cause fetal harm. As a result, Pentacel is not recommended for use in pregnant women. Pentacel is approved for use in infants and children six weeks through four years of age, prior to their fifth birthday. Infants younger than six weeks of age, and children five years of age and older should not receive Pentacel.
- VAXELIS should not be administered to anyone with a history of a severe allergic reaction to a previous dose of VAXELIS, any ingredient found in VAXELIS, or any other tetanus toxoid, diphtheria toxoid, pertussis-containing vaccine, hepatitis B vaccine, inactivated poliovirus vaccine, or H. influenzae type b vaccine. VAXELIS should not be given to anyone who has suffered encephalopathy within seven days of a previous pertussis-containing vaccine with no other identifiable cause. Anyone with a history of progressive neurologic disorder, including infantile spasms, uncontrolled epilepsy, or progressive encephalopathy should not receive VAXELIS until a treatment regimen has been established and the condition has stabilized. Careful consideration should be given to the benefits and risks of VAXELIS before administering the vaccine to someone with a history of fever at or above 105 degrees F, a hypotonic-hyporesponsive episode, or persistent, inconsolable crying lasting more than three hours within 48 hours after a pertussis-containing vaccine, or who has suffered seizures within three days after a previous pertussis-containing vaccine. A causal relation between tetanus toxoid and both brachial neuritis and Guillain-Barré syndrome has been determined by the Institute of Medicine (IOM). If Guillain-Barré syndrome occurred within six weeks of receipt of a prior vaccine containing tetanus toxoid, the risk for Guillain-Barré syndrome may be increased following VAXELIS. Apnea in infants born prematurely has been associated with the administration of intramuscular injections, including VAXELIS. Administration of this vaccine should only be considered after careful assessment of the infant’s health status, along with the potential risks and benefits of vaccination. VAXELIS is approved for use in infants and children six weeks through four years of age, prior to their fifth birthday. Infants younger than six weeks of age, and children five years of age and older should not receive VAXELIS.
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
What questions should I ask my doctor about the Hib vaccine?

NVIC’s If You Vaccinate, Ask 8! Webpage downloadable brochure suggests asking eight questions before you make a vaccination decision for yourself, or for your child. If you review these questions before your appointment, you will be better prepared to ask your doctor questions. Also make sure that the nurse or doctor gives you the relevant Vaccine Information Statement (VIS) for the vaccine or vaccines you are considering well ahead of time to allow you to review it before you or your child gets vaccinated. Copies of VIS for each vaccine are also available on the CDC's website and there is a link to the VIS for Hib vaccine on NVIC's “Quick Facts” page.
It is also a good idea to read the vaccine manufacturer product insert (in this case, Hib vaccine manufacturer product inserts) that can be obtained from your doctor or public health clinic. Federal law requires drug companies marketing vaccines to include certain kinds of vaccine benefit, risk and use information in product information inserts that may not be available in other published information. Hib vaccine package inserts are located on NVIC's Hib disease and vaccine quick fact page.
Other questions that may be useful to discuss with your doctor before getting a Hib containing vaccine are:
- If other vaccines in addition to a Hib containing vaccines are scheduled for my child at this office visit, am I allowed to modify the schedule so fewer vaccines are given at once?
- What should I do if my child has a high fever or appears very ill after vaccination?
- What other kinds of reaction symptoms should I call to report after vaccination with a Hib containing vaccine?
- If the Hib vaccine doesn’t protect my child, do I have any other options for preventing Hib infection?
Under the National Childhood Vaccine Injury Act of 1986, doctors and all vaccine providers are legally required to give you vaccine benefit and risk information before vaccination; record serious health problems following vaccination in the permanent medical record; keep a permanent record of all vaccines given, including the manufacturer’s name and lot number; and report serious health problems, injuries and deaths that follow vaccination to VAERS.
Remember, if you choose to vaccinate, always keep a written record of exactly which shots/vaccines you or your child have received, including the manufacturer’s name and vaccine lot number. Write down and describe in detail any serious health problems that develop after vaccination, and keep vaccination records in a file you can access easily.
It also is important to be able to recognize a vaccine reaction and seek immediate medical attention if the reaction appears serious, as well as know how to make a vaccine reaction report to federal health officials at the Vaccine Adverse Reporting System (VAERS). NVIC’s Report Vaccine Reactions—It’s the Law webpage can help you file a vaccine reaction report yourself to VAERS if your doctor fails or refuses to make a report.
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
NVIC Press Releases, Statements & Commentaries Related to Hib
.jpg.aspx?width=152&height=205)
The Vaccine Reaction
- Raines, K FDA Approves 6 in 1 Combo Vaccine for Babies The Vaccine Reaction Jan. 3, 2019
- Hammond JR Has the Hib Vaccine Simply Shifted the Risk Burden to the Elderly? The Vaccine Reaction Nov. 15, 2018
- TVR Staff Two Infants and a Toddler in India Die Shortly After Vaccinations The Vaccine Reaction Jul. 9, 2018
- TVR Staff Two Infants in India Die Following Pentavalent Vaccination The Vaccine Reaction Mar. 15, 2018
- Vora P Interview: WHO’s Revised Norms are Allowing the Use of Unsafe Vaccines The Vaccine Reaction Jul. 26, 2017
- La Vigne P ActHIB Vaccine Found to Contain Pieces of Glass Between 2013 and 2015 The Vaccine Reaction Jan. 12, 2017
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
Hib disease and vaccine quick facts
Haemophilus Influenzae Type B (Hib)
- Haemophilus influenzae type b (Hib) is a bacterial infection that can cause severe illnesses in children, including meningitis, epiglottitis, pneumonia, arthritis, and cellulitis;
- Hib meningitis, an infection of the membranes covering the brain and one of the most serious complications of Hib, may occur following an upper respiratory illness. Infection can spread from the sinuses and lungs into the bloodstream and to the brain causing meningitis;
- Hib is spread through person-to-person transmission, mostly through the air. It is often found in the respiratory tracts of adults with no noted symptoms or adverse effects. Hib must enter into the bloodstream for it to cause meningitis or other forms of invasive disease;
- Hib infection more frequently occurs in infants and children under the age of five. Other high-risk populations can include Alaska Natives, American Indians, adults 65 years of age and older, and persons with certain medical conditions, including immunosuppression;
- In general, the transmission of Hib is considered to be limited and when it occurs, it usually affects only close contacts such as household members. Prior to the introduction of the Hib vaccine, most children acquired natural immunity to Hib by the time they were five or six years old.
Hib Vaccine
- There are five different Haemophilus influenzae type b (Hib) vaccines available for use in the United States: ActHIB, Hiberix, PedvaxHIB, Pentacel (Hib vaccine combined with diphtheria and tetanus toxoids, acellular pertussis adsorbed, and inactivated poliovirus), and VAXELIS (Hib vaccine in combination with diphtheria and tetanus toxoids, acellular pertussis adsorbed, hepatitis B, and inactivated poliovirus. The CDC recommends infants receive Hib vaccine at 2, 4, and 6 months of age with an additional booster dose between 12 and 15 months of age. Hib vaccine is also recommended by the CDC for use in older children, adolescents and adults with certain medical conditions, however, no Hib vaccines are FDA approved for use in persons over five years of age.
- Mild side effects such as redness, warmth, or swelling where the shot was given have been reported in connection with administration of Hib vaccines. Systemic reactions, such as fever and irritability can also occur. Severe reactions involving Hib vaccination were reported during pre-licensing clinical trials and continue to be reported to the Vaccine Adverse Events Reporting System (VAERS). These include deaths, anaphylactic reactions, asthma, pneumonia, convulsions, noninfectious encephalitis, acute pancreatitis, peripheral neuropathy, Guillain-Barre syndrome, sepsis, seizures, and cerebral edema.
- All infants and children who participated in Hib vaccine pre-licensing clinical trials also received other vaccines in addition to the Hib vaccine. As a result, it is not possible to determine the specific adverse reaction to monitor for following Hib vaccination. The administration of multiple vaccines also makes it difficult to determine the specific vaccine that might have triggered the reactions reported in both clinical studies and to VAERS.
- Using the MedAlerts search engine, as of March 29, 2024, there have been 93,508 reports of Hib vaccine reactions, hospitalizations, injuries and deaths following Hib vaccinations made to the federal Vaccine Adverse Events Reporting System (VAERS), including 2,927 related deaths, 19,094 hospitalizations, and 1,826 related disabilities. Nearly 85 percent of HIB vaccine-related adverse events occurred in children under three years old. Of the Hib-vaccine related deaths reported to VAERS, nearly 92 percent of the deaths occurred in children under three years of age. Of these reported deaths, 2,177 occurred in infants under the age of 6 months.
- As of April 1, 2024, there had been 179 claims filed in the federal Vaccine Injury Compensation Program (VICP) for injuries and deaths following HIB vaccination, including 34 deaths and 145 serious injuries.
Food & Drug Administration (FDA)
- ActHib (Sanofi Pasteur) - Haemophilus b Conjugate Vaccine (Tetanus Toxoid Conjugate) Product Insert and Licensing Information
- HIBERIX (GlaxoSmithKline Biologicals) Haemophilus b Conjugate Vaccine (Tetanus Toxoid Conjugate) Product Insert and Licensing Information
- PedvaxHib (Merck Sharp & Dohme Corp.) - Haemophilus b Conjugate Vaccine (Meningococcal Protein Conjugate) Product Insert and Licensing Information
- Pentacel (Sanofi Pasteur) - Diphtheria and Tetanus Toxoids and Acellular Pertussis Adsorbed, Inactivated Poliovirus and Haemophilus b Conjugate (Tetanus Toxoid Conjugate) Vaccine Product Insert and Licensing Information
- VAXELIS (MCM Vaccine Company) Diphtheria and Tetanus Toxoids and Acellular Pertussis Adsorbed, Inactivated Poliovirus, Haemophilus b Conjugate Meningococcal Protein Conjugate and Hepatitis B Recombinant Vaccine Product Insert and Licensing Information
Centers for Disease Control (CDC)
- CDC on Hib Disease
- CDC on Hib Vaccination
- Hib Vaccine Information Statement
- Your Child's First Vaccines Vaccine Information Statement
Vaccine Reaction Symptoms & Ingredients
Our Ask 8, If You Vaccinate webpage contains vaccine reaction symptoms and more.
Search for Vaccine Reactions
NVIC hosts MedAlerts, a powerful VAERS database search engine. MedAlerts examines symptoms, reactions, vaccines, dates, places, and more.
Reporting a Vaccine Reaction
Since 1982 the NVIC has operated a Vaccine Reaction Registry, which has served as a watchdog on VAERS. Reporting vaccine reactions to VAERS is the law. If your doctor will not report a reaction, you have the right to report a suspected vaccine reaction to VAERS.
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.
Hib Bibliography & Resource Links
Medical Literature
- Puliyel J, Naik P, Revised World Health Organization (WHO)’s causality assessment of adverse events following immunization—a critique Version 2. F1000Res. 2018; 7: 243.
- Puliyel J, Sathyamala C Infanrix hexa and sudden death: a review of the periodic safety update reports submitted to the European Medicines Agency. Indian J Med Ethics. 2018 Jan-Mar;3(1):43-47
- Puliyel J, Kaur J, Puliyel A, et al. Deaths reported after pentavalent vaccine compared with death reported after diphtheria-tetanus-pertussis vaccine: An exploratory analysis Med J DY Patil Vidyapeeth 2018 May 18; 11(2) 99-105
- Langere JD, de Jonge MI Invasive Disease Caused by Nontypeable Haemophilus influenzae Emerg Infect Dis. 2015 Oct; 21(10): 1711–1718.
- Bamberger EE, Ben-Shimol S, Abu Raya B, et al. Pediatric invasive Haemophilus influenzae infections in Israel in the era of Haemophilus influenzae type b vaccine: a nationwide prospective study. Pediatr Infect Dis J. 2014 May;33(5):477-81.
- Sreedhar S, Antony A, and Poulose N Study on the effectiveness and impact of pentavalent vaccination program in India and other south Asian countries Hum Vaccin Immunother. 2014 Jul 1; 10(7): 2062–2065.
- Amy Blain, Jessica MacNeil, Xin Wang, et al. Invasive Haemophilus influenzae Disease in Adults ≥65 Years, United States, 2011 Open Forum Infect Dis. 2014 Sep; 1(2): ofu044.
- Bergfors E, Hermansson G, Nyström Kronander U et al. How common are long-lasting, intensely itching vaccination granulomas and contact allergy to aluminium induced by currently used pediatric vaccines? A prospective cohort study. Eur J Pediatr. 2014 Oct;173(10):1297-307.
- Salimnia H, Lephart PR, Asmar BI, et al. Aerosolized Vaccine as an Unexpected Source of False-Positive Bordetella Pertussis PCR Results. J Clin Microbiol. 2012 Feb; 50(2): 472–474.
- Giufrè M, Cardines R, Caporali MG et al. Ten years of Hib vaccination in Italy: prevalence of non-encapsulated Haemophilus influenzae among invasive isolates and the possible impact on antibiotic resistance. Vaccine. 2011 May 17;29(22):3857-62
- Rubach MP, Bender JM, Mottice S et al. Increasing Incidence of Invasive Haemophilus influenzae Disease in Adults, Utah, USA Emerg Infect Dis. 2011 Sep; 17(9): 1645–1650.
- Bender JM, Cox CM, Mottice S, et al. Invasive Haemophilus influenzae disease in Utah children: an 11-year population-based study in the era of conjugate vaccine. Clin Infect Dis. 2010 Apr 1;50(7):e41-6
- Adam HJ, Richardson SE, Jamieson FB et al. Changing epidemiology of invasive Haemophilus influenzae in Ontario, Canada: evidence for herd effects and strain replacement due to Hib vaccination. Vaccine. 2010 May 28;28(24):4073-8
- Murphy TF, Faden H, Bakaletz LO, et al. Nontypeable Haemophilus influenzae as a pathogen in children. Pediatr Infect Dis J. 2009 Jan;28(1):43-8
- McConnell A, Tan B, Scheifele D, et al. Invasive infections caused by haemophilus influenzae serotypes in twelve Canadian IMPACT centers, 1996-2001. Pediatr Infect Dis J. 2007 Nov;26(11):1025-31.
- Zinka B, Rauch E, Buettner A, et al. Unexplained cases of sudden infant death shortly after hexavalent vaccination. Vaccine. 2006 Jul 26;24(31-32):5779-80.
- Millar EV, O'Brien KL, Watt JP, et al. Epidemiology of invasive Haemophilus influenzae type A disease among Navajo and White Mountain Apache children, 1988-2003. Clin Infect Dis. 2005 Mar 15;40(6):823-30.
- Sarangi J, Cartwright K ,Stuart J et al. Invasive Haemophilus influenzae disease in adults. Epidemiol Infect. 2000 Jun; 124(3): 441–447.
- Karnoven M, Cepaitis Z, Tuomilehto J. Association Between Type 1 Diabetes and haemophilus Influenzae Type b Vaccination: Birth Cohort Study. BMJ. May 1, 1999. 318(7192), 1169-1172.
- Urwin G, Krohn JA, Deaver-Robinson K, et al. Invasive disease due to Haemophilus influenzae serotype f: clinical and epidemiologic characteristics in the H. influenzae serotype b vaccine era. The Haemophilus influenzae Study Group. Clin Infect Dis. 1996 Jun; 22(6):1069-76.
- Adams WG, Deaver KA, Cochi SL, et al. Decline of Childhood Haemophilus Influenzae Type b (Hib) Disease in the Hib Vaccine Era. JAMA. 1993 Jan 13;269(2):221-6.
Media Articles
- Di Filippo E 'We've been in such shock': 35-year-old Canadian woman dies from rare bacterial infection Yahoo News Dec. 11, 2018
- Puliyel J ‘Vaccine killing children instead of protecting them' TSG Sunday Guardian Live Mar. 18, 2018
- Kennedy S. No recall for glass found in vaccines made in Monroe County. The Morning Call Dec. 10, 2016
- Express News Service More children died after getting Pentavalent vaccine than DPT, says study The New Indian Express Mar. 16, 2018
- Fierce Pharma FDA approves expanded use of GSK Hib vaccine from booster dose to full series Press Release Jan. 19, 2016
- Devraj R Doctors Resist Deadly Vaccine Inter Press Service News Agency Feb 8, 2014
- Varshney V. Vaccine Woes Continue. Down to Earth. March 12, 2012.
- Kaur R. Officials Push Five-in-One Vaccine. Down to Earth. July 31, 2010.
- Lavenda L. U.S. FDA Licenses Sanofi Pasteur's New Pediatric Combination Vaccine, Pentacel. Eurekalert. Jun. 23, 2008.
IMPORTANT NOTE: NVIC encourages you to become fully informed about Haemophilus Influenzae Type B (Hib) and the Hib vaccine by reading all sections in the Table of Contents, which contain many links and resources such as the manufacturer product information inserts, and to speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child. This information is for educational purposes only and is not intended as medical advice.



